Osteoarthritis is the most common type of arthritis, which we often refer to as “wear and tear”. More recently, the more optimistic “wear, tear, and repair” has been the explanation of choice. It’s a normal age related change like grey hair or wrinkles. For a lot of people it won’t cause any symptoms, and it is not considered a rheumatological condition.
Any joints with cartilage in them can develop osteoarthritis, but some joints that are more often affected include the knee, hip, and hand joints. The process is simply a degeneration of the cartilage covering the bones in the joint. If it occurs in the spine it is also known as “spondylosis” or “spondyloarthritis”.
As mentioned above, osteoarthritis can occur without any symptoms, or there may be some pain or crunchiness in the joint. In the later stages, the joint may start to lock or give way. Osteoarthritis is the most common cause of knee and hip replacements.
But there is good news! Although many people think that arthritis means they’re going to have to put up with their symptoms until they can get a joint replacement, arthritis can be very responsive to osteopathy. Before it gets to a later stage, all the joint wants is movement.
The Process of Osteoarthritis
Cartilage does not have a good blood supply. This means that it is relatively difficult to get rid of waste products and bring in nutrients. You can think of a cartilage as like a sponge, sitting in a bowl of clean water. The water plays the role of the fluid within the joint. If the sponge is full of waste fluid, very little will spontaneously leave the sponge without movement. But if you can compress and decompress throughout the sponge, the waste will start to flush out and the fresh water will take its place.
Still thinking about the sponge analogy, use a hip joint as an example. Think about how the joint moves when you walk. Bringing the leg forwards will compress some of the joint and allow the rest to decompress, and bringing it all the way back will do the opposite. If you were to start shuffling and taking shorter strides, then some of this cartilage will be under more pressure, and other areas may never be compressed. This is one opportunity for osteoarthritis to begin- “use it or lose it” is a good mantra here!
Overuse or misuse of a joint can also lead to osteoarthritis, which makes sense when you think about the example above. Over-compression in one area and under-compression elsewhere is not good for the joint.
The Pathophysiology of OA
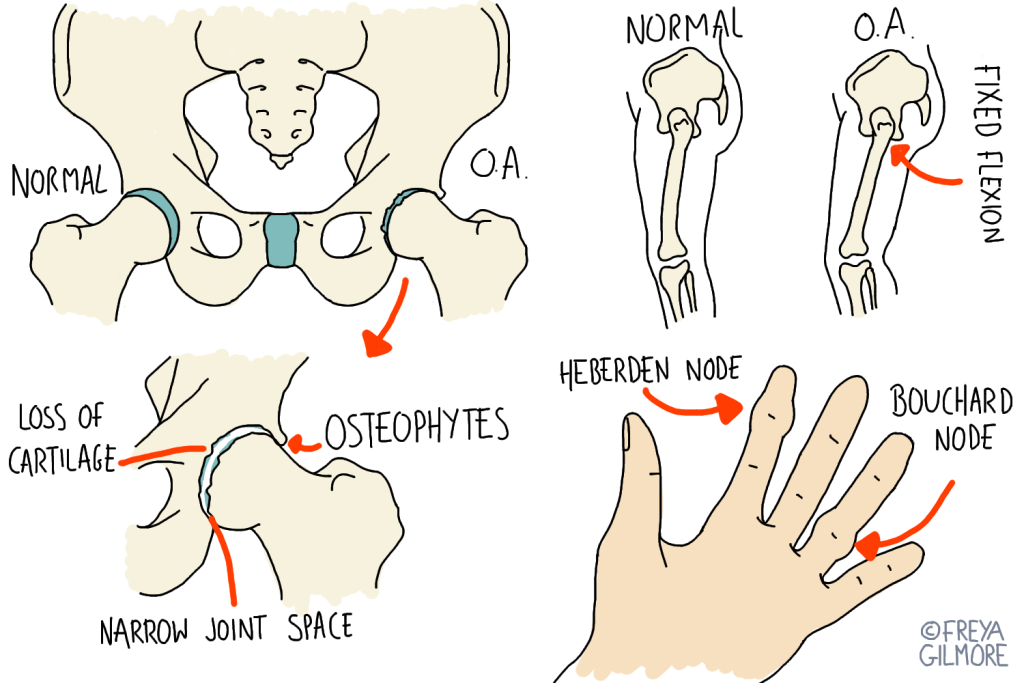
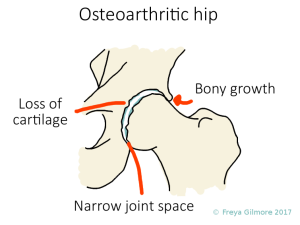
This helps to explain the symptoms some might feel if they have osteoarthritis. As the joint surface becomes more rough, movement can become more crunchy. Locking can be caused by loose bodies of cartilage in the joint, or the bony growth (called osteophytes) that forms to both fill the space left by lost cartilage and in an attempt to stabilise the joint. This occurs in more advanced stages of osteoarthritis. Unfortunately, these natural responses do not help improve movement: and movement is what we need to get the fluid exchange through the cartilage.
Specific Osteoarthritis symptoms by joint
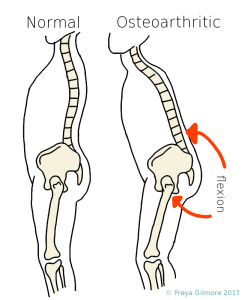
More specifically, an osteoarthritic hip is often stuck in a slightly flexed (forward) position. This means that strides are normally shorter and the body may have to compensate for lost movement elsewhere. The lower back and neck commonly make up for this change. This is the stereotypical “elderly” posture, so keep your hips moving!
The small joints in fingers can be visibly affected, becoming stiff and appearing swollen. These swellings are called Herberden or Bouchard nodes depending where they form. These terms are only used for osteoarthritis (not other causes of swelling) but do not constitute a diagnosis in themselves. Other conditions can appear similarly, so it’s best to have any changes looked at.
What can be done to avoid or delay surgery?
As with most causes of pain, we need to address it from a few different angles:
Mechanically, we want to get the joint moving as well as we can. In treatment this means coaxing the joint into the movement, and loosening off tight muscles that are restricting it. Daily exercises to keep that range of movement and to get more out of it between sessions are also really important.
But we also need to address the way a patient thinks about their pain. It’s quite possible that the arthritis developed after a twinge of pain made them adapt to avoid it. A lot of patients mention that they are worried that they will cause further damage in their daily activity. This is very rarely the case, and even just being told this can make an instant change!
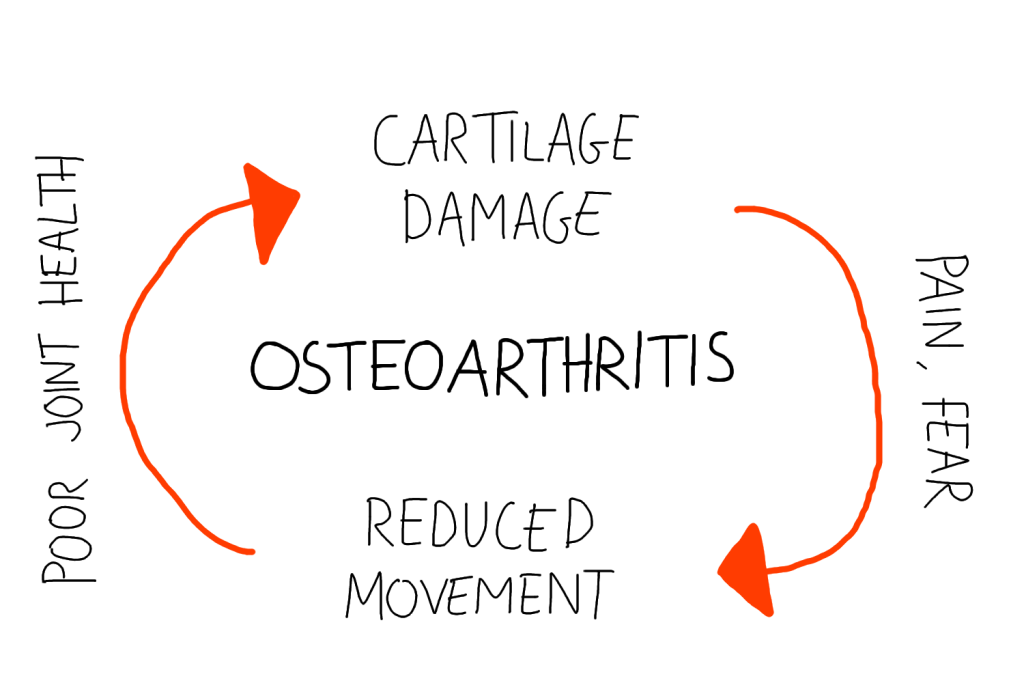
Pain does not always equal harm, and an osteopath can help find the right range. Understanding that you are safe to move is the first step in changing the habits that can make or break your osteoarthritis progress.
For some cases, surgery will be unavoidable. But even if the arthritis itself is not managed by osteopathic treatment, there is still a benefit in “prehab” for the area. The more healthy and strong you are before surgery, the better you will recover.
Research and testimonials
Osteopathic treatment will not cure arthritis, but we know that it can improve the symptoms of it.
“After my first treatment with Freya I felt like I’d had a brand new spine fitted. Movement I’d assumed was becoming limited through age is suddenly not just possible but easy. I can’t recommend her enough – she listens to what’s causing you trouble and then thoroughly investigates the problem.”
Patient Testimonial: P.S. 2017
Click here to make an appointment for your osteoarthritis in Milton Keynes or Buckingham