Osteopaths are qualified to help manage your rheumatic pain. As rheumatic conditions are autoimmune, medication is often a key part of management, as we cannot address the root cause. However, we can help to counteract the way the body reacts to elements of the condition. This includes treatment for the joints that are directly affected, but also to areas that work differently to compensate for them.

This post covers two relatively common rheumatic conditions: Ankylosing Spondylitis (AS/AxSpA) and Rheumatoid Arthritis (RA). It’s a long post, so click here to skip down to RA.
AxSpA & AS (Ankylosing Spondylitis)
AxSpA is an abbreviation of Axial Spondyloarthritis. It may also go by AS, although this is more commonly used for ankylosing spondylitis. AxSpA literally means “spinal arthritis”, but the condition is more specific than that.
It is a very under-diagnosed inflammatory condition, in the rheumatic family of autoimmune diseases like rheumatoid arthritis and Crohn’s disease. It has a strong genetic component, meaning that it is not a result of injury or posture. Symptoms usually begin in the teenage years with the average age of diagnosis being 24, most patients have experienced symptoms for at least 8 years before a correct diagnosis.
People with AxSpA will likely find that they:
- Gradually developed lower back pain over weeks or months and remained for at least 3 months
- Have lower back pain that is worse after rest and takes a while to get going
- Feel better after anti inflammatory medications (NSAIDs) and activity
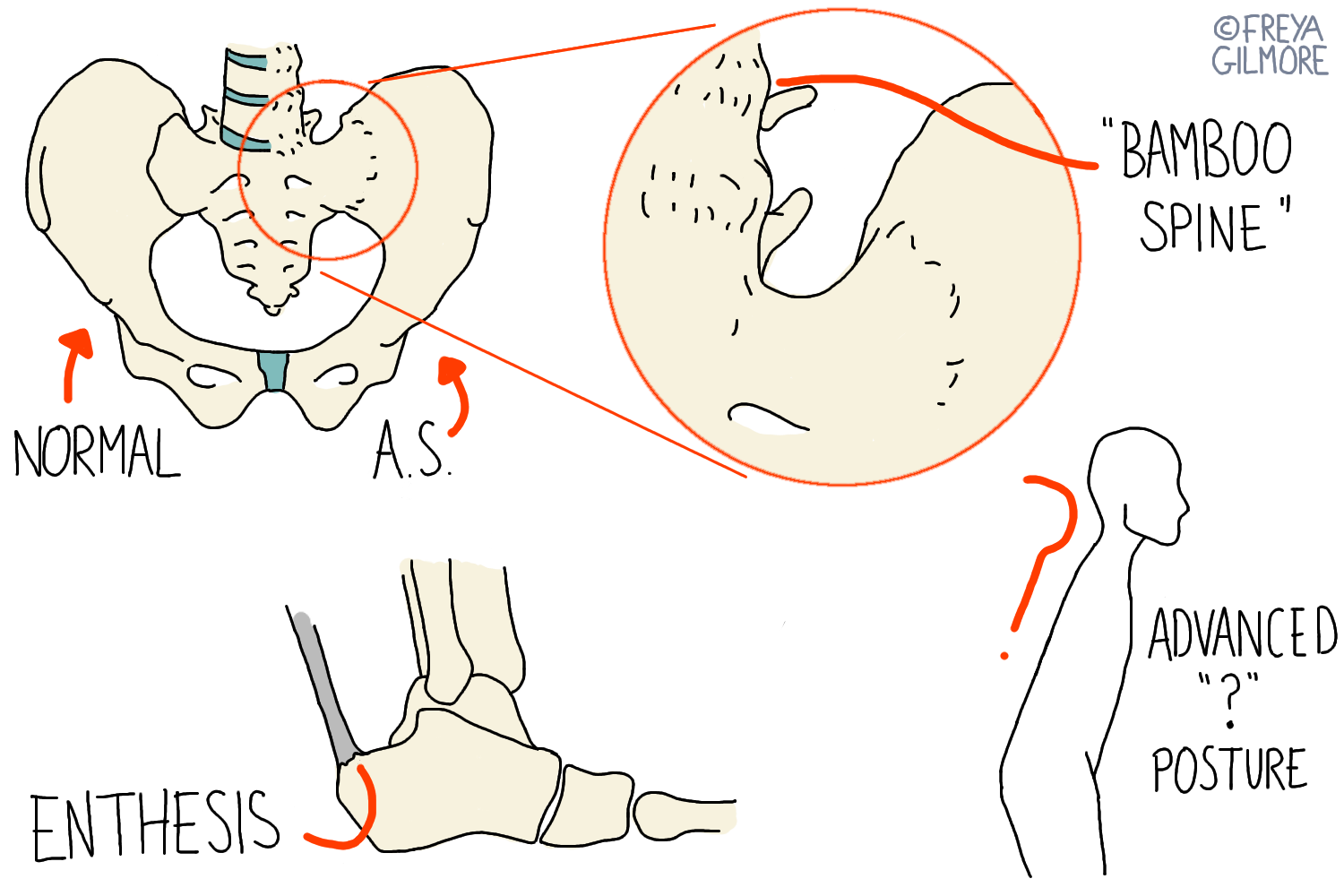
- Are prone to tendon problems like Achilles tendinitis
Other signs can include:
- Recurrent uveitis (eye inflammation, not infection)
- Repeated episodes of costochondritis
- inflammatory bowel diseases
- Fatigue
- Night sweats or pain in the second half of the night
- Psoriasis
Ankylosing Spondylitis
Ankylosing Spondylitis (AS) is a more severe, later stage form of AxSpA, when changes are visible on X-ray. The name means “fusion and inflammation of the spine”. In this condition, the joints of the spine and pelvis become inflamed, and the body reacts to this by laying bone down over the joint. This causes pain and loss of movement through the lower back. Not all people with AxSpA will develop AS.
It was previously thought that AS was easy to spot because of the “question mark” shaped posture. We now know that this posture is the effect of badly managed AS.
Changes on x-ray are more obvious with men than women, which means that AS is more commonly diagnosed in men than women. However AxSpA affects both sexes equally.
Diagnosis of AxSpA and AS
Full diagnosis of either AxSpA or AS requires a rheumatologist, but anyone can spot the signs using the Spade Tool.
Blood tests may be the first test that will be done. Expect signs of inflammation: raised CRP and ESR- although it is possible to have AxSpA without these signs. 90% of people with AxSpA will have the HLA-B27 gene. Around 8% of the population have this marker and only 1% of these people will develop AxSpA; therefore this is not a useful test for routine screening but is very helpful if AxSpA is suspected. You can be HLA-B27 negative and still have AS.
AS will show up on x-ray. 7/10 of people with AxSpA who don’t have changes on x-ray will have changes on MRI.
Management of AxSpA and AS
AxSpA and AS cannot be cured by osteopathy. Manipulation is not appropriate in any instance due to fusions and potential damage to bones. The bone that forms over these joints is weak, and fracturing it is not a solution. Generally strong treatment can also lead to a strong treatment reaction, “micro treatments” may be of more benefit. As manual therapy may lead to flairs in symptoms its important to carefully manage any treatment plans.
Osteopathy can help to manage the symptoms on a temporary basis. Gentle work to maintain movement and pain relief is useful. Prescription of appropriate exercises to continue the benefit at home are also important- particularly establishing a routine for bad days. Educating the patient to give them the power to speed up their diagnosis and understand their options are arguably the most valuable thing an osteopath can offer a patient with suspected AxSpA.
Medication is important: stronger anti-inflammatory drugs can make a big difference. If response is not as desired, the rheumatologist may recommend Biologics such as Anti TNF: stronger drugs that compromise the immune system, thus reducing the disease activity.
Andrew

Andrew is an osteopath who has AS. On a bad day he has very reduced movement first thing in the morning, but with five minutes of gentle treatment, his pain is reduced and his movement is improved enough that he can work.
His AS was diagnosed after roughly 15 years of disease progression. This picture taken shortly after diagnosis shows that the textbook image of a “?” posture is not accurate. Andrew still enjoys weight training when his symptoms are under control.
Without Freya I would not still be able to work. She keeps me able to go to the gym and manage my symptoms.
Alongside clinical work, Andrew works in research at the University College of Osteopathy. He has a paper published in the International Journal of Osteopathic Medicine (IJOM) on the topic of AxSpA.
Mental Health and AxSpA and AS
People with AxSpA or AS are at higher risk of mental health problems. 59% of patients suffer from mental health problems, compared to 25% of people with chronic back pain, and 5% of the general population.
Speaking to your GP is a good place to start for accessing mental healthcare, but the service is very oversubscribed. Other routes include directly contacting a local counsellor, or reaching out to charities such as the Samaritans or Mind.
Other Resources
ASone is a site designed for younger people with AS.
NASS is a charity looking to improve care for people with AxSpA. They are interested to see the diagnosis process, so if you are undergoing testing for AxSpA, get in contact with them.
My AxSpA app for tracking symptoms & social network
Rheumatoid Arthritis
Rheumatoid Arthritis is another inflammatory form of arthritis, typically affecting small joints first. Hand, foot, and neck symptoms may be the first to arise. It is often confused with osteoarthritis, but the two are very different.
RA Disease Process
RA is an autoimmune condition, meaning the body attacks its own tissues. Different rheumatic conditions affect different tissues, and for RA the target is a layer of tissue within joints- the synovium. There are a few variations in the way the disease can behave, but most commonly, it will follow a relapsing and remitting pattern. During a flare, affected joints will become inflamed and painful
Read more about hand exercises for RA and watch the video demonstration here.
Make an appointment in Buckingham or Milton Keynes to manage your rheumatic pain