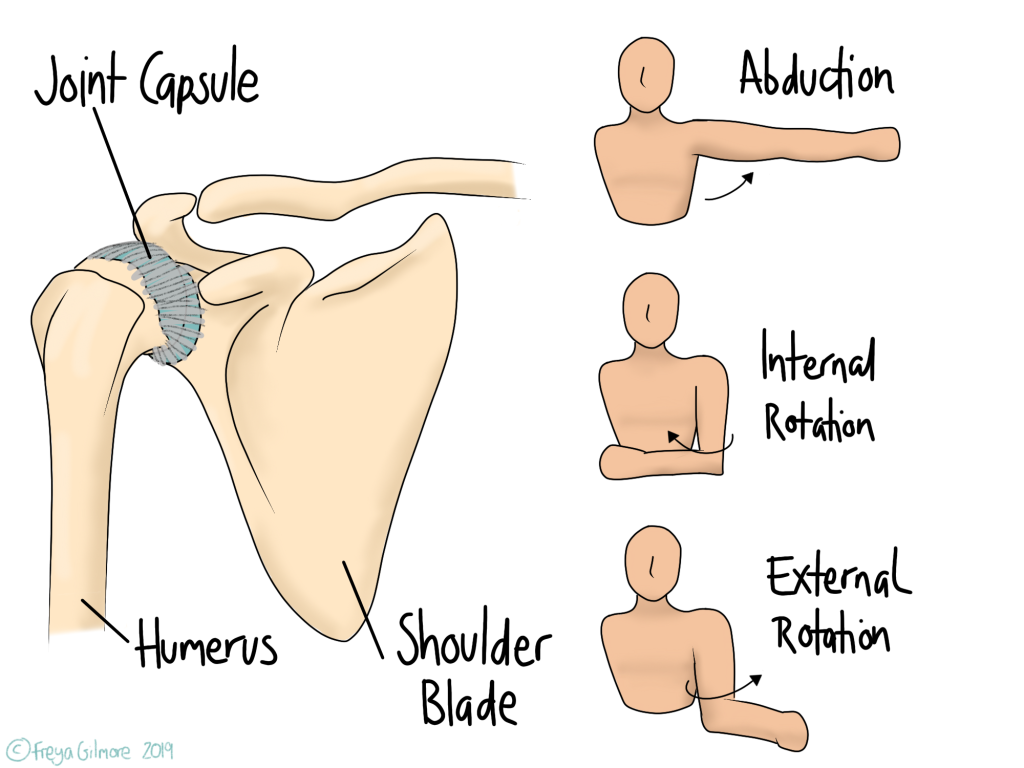
Frozen shoulder (FSS) is a syndrome, meaning it is defined by its signs and symptoms. Typically someone with a frozen shoulder will have pain and stiffness in the shoulder, but the diagnosis only applies to people whose movement is restricted passively. This means that when the shoulder is relaxed, movement is still limited when someone else is performing the movement.
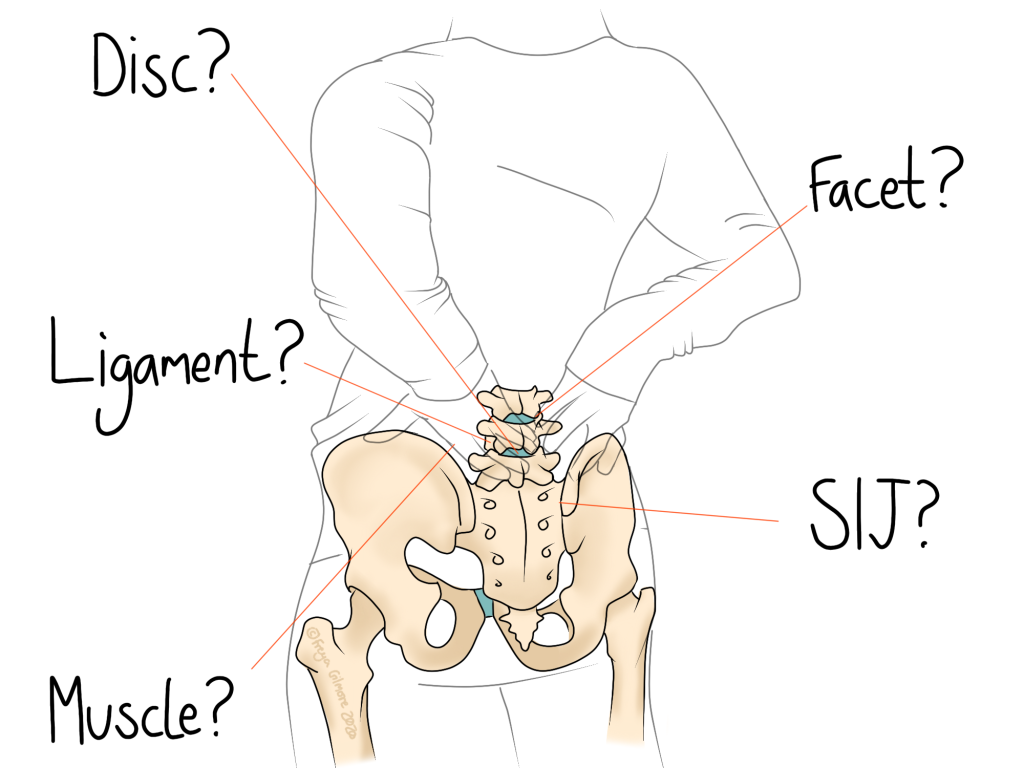
There are other causes of lost passive movement in the shoulder, so your osteopath will rule these out before making a diagnosis. They may want you to see your GP to arrange an x-ray to rule out other conditions.
The name “adhesive capsulitis” means “sticky and inflamed capsule”, in reference to the joint capsule. The joint capsule is connective tissue that surrounds the joint. It is not entirely known what happens within the joint in frozen shoulder, but the current idea is a mix of inflammation within the joint, and a thickening of the joint capsule.
There are three phases in the cycle of frozen shoulder:
- Freezing phase
- Frozen phase
- Thawing phase
The duration of each stage varies a lot. Commonly quoted figures from start to finish range from 10 months to over 4 years. It appears that the process can be sped up by interventions such as manual therapy, exercise, or injections. Osteopathic treatment encompassing not just the shoulder but also the neck and upper back have a positive effect on FFS.
Freezing
- Movement becomes restricted
- Pain is at its worst
Frozen
- Movement is most restricted
- Pain subsides
Thawing
- Pain and lack of movement begin to resolve
What causes Frozen Shoulder?
There are two categories of frozen shoulder: primary and secondary.
Primary FFS appears without warning, not following any trauma or other explanation for the syndrome. In these cases, it is unclear what causes the condition. Secondary FSS follows a significant event such as an injury or immobilisation, or coincides with another condition such as diabetes or high blood pressure. People with diabetes are twice as likely to develop FSS than people who do not have diabetes. It is not uncommon for the other shoulder to freeze a few months after the first resolves.
It appears that there are a number of factors that make a person more likely to develop frozen shoulder, but what initiates the process is largely unknown. Along with conditions listed as causes of secondary FFS, connections have been made with:
- Thyroid problems
- Parkinsons disease
- Problems with the joints in the neck
- Some forms of heart disease
What can be done?
As mentioned above, manual therapy such as osteopathy has been shown to have positive effects on the duration of frozen shoulder episodes. Exercise is also important for continued progress. As there are links between FFS and inactivity, exercise may prove to be a good preventative strategy for new episodes of FFS.
As FFS is such a slow condition to resolve, it is recommended that full investigation is conducted, included imaging if deemed appropriate. Your osteopath will be able to guide you through recovery and refer back to your GP if progress is inadequate or you decide to investigate interventions such as surgery or injection.
Click here to book an appointment for your frozen shoulder in North Bucks