Diagnosing someone with hypermobility is essentially a fancy way of saying they’re more bendy than most, or “double jointed”. It is not a problem by default, but it can cause aches and pains. These symptoms tend to improve with rest, and are aggravated by exercise- although strengthening exercises can be a useful management strategy.
Hypermobility is essentially laxity of ligaments. Ligaments are there to stop joints from bending too far, so if they’re not doing their job, the muscles can take over. Keeping those muscles strong means they can work efficiently and don’t have to overwork on a daily basis.
BHS is more common in women than men, and decreases with age. It is not inflammatory and does not progress.
Beighton Score
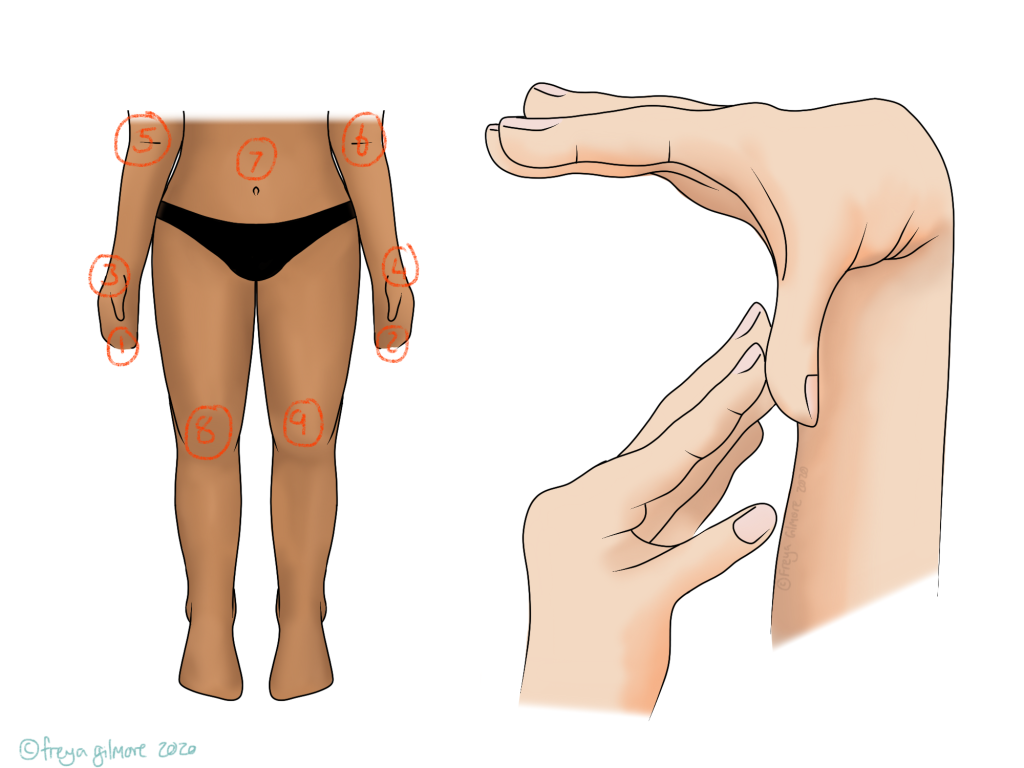
The Beighton score is used in conjunction with other factors to determine whether or not a diagnosis of BHS is appropriate. It is not exhaustive, but can be a good starting point.
- A point for bending fingers back to 90 degrees on each hand (1, 2)
- A point for bending each thumb to reach the wrist (3, 4)
- A point for extending each elbow beyond neutral (5, 6)
- One point for bending forward with locked knees and touching the floor (7)
- A point for straightening each knee past neutral when standing (8, 9)
Other Features of Benign Hypermobility Syndrome
When diagnosing BHS, other factors are taken into account along with lax joints themselves. Chronic pain, particularly in more than one joint can point towards BHS, as can things like bursitis and epicondylitis (tennis/golfers’ elbows). Multiple dislocations (in the same joint or not) are also a consideration for diagnosis.
When is hypermobility not benign?
Benign hypermobility syndrome does not include systemic rheumatological disease. Examples of rheumatological diseases that are linked to hypermobility include some types of Ehlers Danlos Syndrome (EDS), Marfan Syndrome, and Osteogenesis Imperfecta (“brittle bone disease”).
There are also other causes of joint pain and laxity that your osteopath may want to send you for a blood test to rule in or out.
As mentioned above, joint laxity due to trauma is not the same as benign hypermobility, although similar management can be useful.
Hypermobility and Osteopathy
Very rarely does a patient come into clinic complaining of hypermobility. It’s more likely that they have symptoms such as achey muscles around a hypermobile area. Less commonly, patients book in to manage their recurrently dislocating joints, such as a shoulder. If the cause of a recurrent dislocation is traumatic, the ligaments will be lax, but that does not mean the patient necessarily has BHS. The same goes for ankle laxity after a bad sprain.
Your osteopath can recommend exercises to strengthen the muscles in question, as well as helping the rest of the body ease the load on the affected joints.
Book an appointment here to assess and manage your hypermobility in Milton Keynes or Buckingham